Aquaporin-4, a mysterious new suspect in depression
- Oktay Genel

- Nov 25, 2021
- 5 min read
Updated: Jan 25, 2023
I am a London-based medical student, currently taking a master’s degree in Neuroscience at the Institute of Psychiatry, Psychology and Neuroscience (IoPPN), home to the Stress, Psychiatry and Immunology (SPI) lab. While it may seem rather unusual for a medical student to stick his nose into the complexities of the biology of depression, one title among our list of Year 3 research projects particularly caught my attention: “The role of Aquaporin-4 (AQP4) in the pathogenesis of depression”. How important could the role of this basic protein be in such a complex disorder like depression?
In this blog, we are going to have a look at some of the findings from our research on this topic. I will start by explaining the importance of AQP4 in the pathology of depression, then summarise findings from animal and human studies, briefly explore the role of autoimmunity and conclude by reporting the relevance of our work to patients with depression.
Aquaporins, otherwise known as water pores or channels, are very tiny gates embedded into the outer membrane of a cell. Their function is to control the amount of water either going outside, or coming inside the cell, like a border police officer.

There are many different types of aquaporins in the body, actually about a dozen, which all serve a specific function. For instance, it is known that the first-ever discovered aquaporin, AQP1, is essential to make urine more or less concentrated in the kidney.
The same principle occurs in the brain, where the most common aquaporin is AQP4. In an immensely complex organ such as the brain, made of around 75% water, it seems highly possible that a disruption in the organisation of water could disrupt the brain’s function as well. Given that brain function is known to be impaired in depression, we had to know whether AQP4, the brain’s “Minister of Water”, really had a role in the development of this serious psychiatric condition. To do this, we conducted a review of the literature. This means that we looked at all existing research articles on this topic to try to make conclusions.
The link between stress, inflammation, depression and AQP4
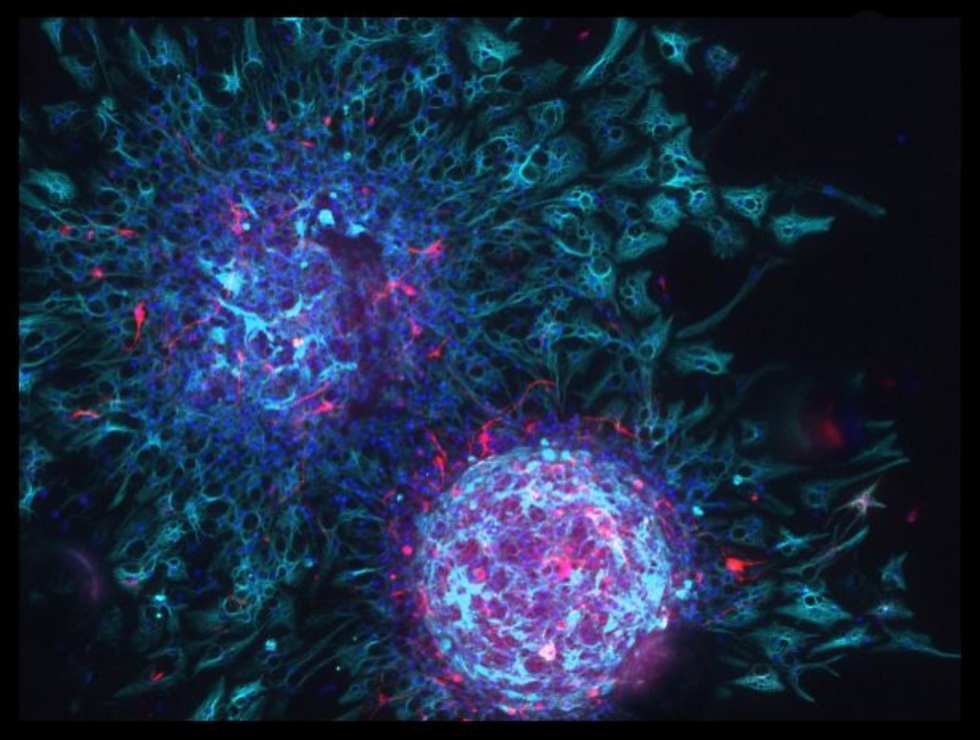
It has been known for a while now that both stress and inflammation are important parameters in depression. One possible way for stress and inflammation to cause this condition is through decreasing neurogenesis, the formation of new neurons (brain cells), in critical areas of the brain. The decrease of neurogenesis is very strongly implicated in depression.
Interestingly, more evidence has recently shown that AQP4 has a role in the regulation of stress, inflammation and importantly, neurogenesis!
This is why we wanted to take a step back to summarise the link between AQP4 and depression.
Animal studies
First of all, we looked at studies performed on mice exposed to stress or inflammation, which reported the change in AQP4 levels before and after the exposure. There are several established protocols and conditioning experiments which can be used to induce stress or inflammation in mice.
What about the results? Exposing animals to stress and inflammation usually decreased the levels of AQP4 in their brains. This decrease happened in the cortex, but also in the hippocampus, the region of the brain where neurogenesis is known to take place… Moreover, injecting anti-depressant medication to animals restored their AQP4 levels.
But what role exactly does AQP4 play in the brain? The best way to understand the importance of something is to take it away. If you want to know the role of salt, try cooking without any. In the same way, to understand the role of AQP4, the best way is to produce an animal which does not have any AQP4 in its brain. This is what we call a “knock-out”, carried out using genetic techniques.
From these studies, we understood that AQP4 acts sort of like a shield, protecting against the depression-causing effects of inflammation on brain cells. While AQP4 did not protect against the effects of psychological stress, it was necessary for the action of anti-depressants.
Human studies
The next step was to look at the role of AQP4 in more “real life” situations, from studies using human tissue. There were three types of studies in this case: some studies using brain tissue from deceased patients, some using brain tissue collected from neurosurgery, and some studies using patients’ blood. In all of these studies, the main idea was to compare AQP4 levels in individuals with or without depression.
In tissue from deceased patients and from surgery, AQP4 levels were significantly lower in depression patients. Guess where? Again, especially in the hippocampus. However, in blood tissue, no difference in AQP4 levels was observed between patients with depression and individuals without depression. This finding needs to be taken with caution, given that AQP4 is also generally less expressed in places other than the brain.
Autoimmunity
Autoimmunity refers to the targeting and destruction of good cells by our immune system, which mistakenly believes them to be bad cells. This is the basis for many serious diseases, such as type 1 diabetes. Another autoimmune disease, called neuromyelitis optica or Devic’s disease, is caused by a wrong targeting of AQP4 in the eye nerves, thereby affecting vision. We wanted to know whether a similar event happens in depression, in which the wrong targeting of AQP4 could be causing depression.
Only two studies have investigated autoimmunity towards AQP4 in the context of depression. None of the patients had AQP4 auto-antibodies. It is very difficult to draw meaningful conclusions from such a little number of studies, especially given that the first one only included a single patient, who developed symptoms of neuromyelitis optica later. More work is needed to determine if AQP4 autoimmunity really has a role in depression.
Ok but why is this so important?
In our review, now published in Brain, Behavior, and Immunity, we open the door for a new area of research, which could help us further understand the link between AQP4 and depression. In summary:
In animals we found that biological and psychological stress, as well as inflammation, decrease brain AQP4 expression, and that AQP4 prevents the effects of stress and inflammation on depression-causing mechanisms.
In humans, AQP4 is decreased in the brain tissue, but not the blood tissue, of patients with depression. Autoimmunity towards AQP4 does not seem to be really implicated at this stage.
This means that AQP4 could be used as a therapeutic agent in order to protect the brain from depression!
While it is known to be difficult to modify genes in humans to make them produce more of a molecule (gene therapy), it is an interesting avenue to explore, which could yield highly positive results for patients.
Wishing everyone high levels of AQP4 water channels!





