The Future is Feminist: tackling gender inequalities in psychiatric medicine and practice
- Rebecca Murphy Lonergan

- Sep 3, 2020
- 6 min read
Special note from the editors: This is the fourth blog of our new series, The future of mental health as seen by the future leaders in mental health, written by the 2020 ‘Psych Stars.’ Selected by The Royal College of Psychiatrists, Psych Star ambassadors are a group of final year medical students awarded for their particular interest and commitment to psychiatry. During the year-long scheme as Psych Stars, students are nurtured in their interest in psychiatry through the assignment of mentors, by gaining access to learning resources and events, and by becoming part of a network of like-minded students. More information on the Psych Stars scheme can be read here. We have decided to invite each of the Psych Stars to write a blog on how they envision the future of mental health by choosing an area in which they are passionate. We have decided to run the series as a celebration of these student’s success and to provide an outlook for each of the awardees to share their passion. With a new blog published each Friday, the series will run over the next few months.
Psychiatry, like most scientific and medical fields, has historically not been kind to women. Freud himself, still heralded by some as the father of modern psychiatry, considered women to “oppose change, receive passively, and add nothing of their own”, a perception that half the population has not necessarily been able to shake since.
While in some respects Freud’s acknowledgement of women’s sexuality were remarkably progressive for the era, his somewhat obsessional emphasis on labelling these desires as hysterical and rooted in a woman’s aspirations to be more like her male counterpart were less welcoming, and was coupled with fashion of the time for lobotomy, incarceration and sterilisation to manage “perverse sexual misbehaviour”.
Underlying these views, however, was a desire to understand what Freud considered unfathomable — untangling the “riddle of femininity” and women, who were notably absent from the medical profession until the late 1800s — something Freud declared beyond even the power of his superior male brain.

As a student at Edinburgh Medical School, the first UK institution to accept female students, I am exceptionally proud of the university’s legacy and contribution to the empowerment of women, particularly in medicine. However, my own experiences of sexism and those of my peers, both in a clinical and teaching environment, have exemplified to me the need to continue to strive and campaign for equality.
It was only more recently that I began to explore how the underlying sexism in medical literature and the education and treatment of women students might also be affecting patient care, which is described extensively in Caroline Criado Perez’s 2019 book, Invisible Women. Organisations such as the Medical Women’s Federation and the Women in Healthcare Leadership project have created vital platforms and communities for women doctors to share experiences and support a new generation of medical graduates, whom may be better prepared to tackle prejudices and reshape future practice to overcome some pitfalls discussed here.
By the 21st century, the medical field has managed to debunk some of Freud’s more divisive theories on women.
Modern Psychiatry boasts an impressive proportion of women physicians, academics and allied health professionals, when compared with most surgical and internal medical specialties. Currently, women make up the majority of medical students, the majority of junior doctors and the majority of psychiatry trainees. Notable leadership and management roles in Psychiatry are or have recently been occupied by women, including past College Presidents. Therefore, one could be forgiven for presuming that the patriarchy has been thoroughly dismantled in some, if not all, fields of medicine.
But how does this relate to patient care?
Representation, within doctors and other healthcare staff, is crucial to delivering person-centred care as it increases the diversity of opinion and insight into a patient’s wellbeing. To match the diversity of patients within psychiatry requires the same level of diversity of ethnicity, religion, disability, and sexual orientation as well as gender in order to understand similarities between lived experience.
From a patient perspective, however, it might not quite be time to pat ourselves on the back for a jolly good job well done.
The evidence suggests that, in many respects, psychiatry, much like other fields of medicine, is still failing women. Incarceration and lobotomy aside, our inherent biases shaped by gender stereotypes insidiously invade aspects of medical practice and may contribute to a gender care gap.
Women, as the quintessentially more “emotional sex”, are diagnosed with depression or anxiety nearly twice as often as men, and are twice as likely to be on an anti-depressant, even when they have not reported depression in the consultation. This is often attributed to health-seeking behaviours, with more women than men consulting their GP, and the assumption that women are generally more comfortable discussing their mental health. However, there are studies of note which have actually found lower rates of depression in women and yet still higher rates of anti-depressant prescribing.
More sinister, however, are the number of testimonies from women whose physical symptoms indicative of an underlying organic health condition were disregarded as psychosomatic (physical manifestations of psychological upset) or stress-related — the equivalent of sending your male patient with abdominal pain for a CT scan whilst reassuring your female patient that she probably needs to relax more and ‘it’s all in her head anyway’.
This mimics studies which previously found that, in response to pain, men were more likely to be offered painkillers and women, antidepressants or sedatives drugs such as diazepam.
Our implicit biases, carried by both men and women physicians, which may still consider the behaviours of women to be more irrational and hyperbolised, demonstrate that the sole presence of women within a professional field is not enough to grant equal representation and, moreover, representation is not enough to power definitive change of attitude. Alternatively, we may just not account for the possibility that men and women experience pain and ill-health differently.
Looking forward, as we teeter on the precipice of an impending COVID-related global mental health crisis, we are granted a unique opportunity to assess our circumstance and determine the direction we take from here.
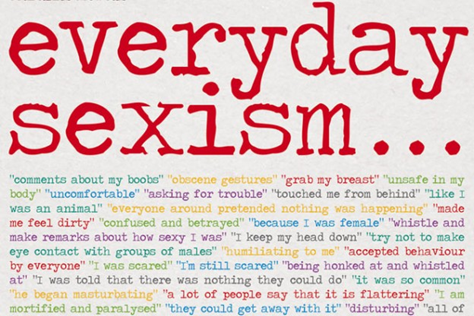
Feminism is able to monopolise on large waves of change, from the success of the #metoo movement, the everyday sexism project and acceptance of intersectional feminism into youth culture, thanks to role models and advocates like Michelle Obama, and as such, the political unrest in the aftermath of the coronavirus pandemic should be no exception.
There are several key areas than warrant address with regards to medical feminism.
Firstly, there is need to tackle the major data gaps in psychiatric research, including within drug manufacture and trials, all of which historically forget women: the vast majority of pre-clinical in vitro and animal studies use only male test subjects, and, those that do, rarely sex-disaggregate data, even in female-prevalent conditions, such as the development of novel anti-depressants. In addition, we need to reassess how our epidemiological data, looking at the distribution of illness, considers gender, as an independent risk factor determined by chromosomal composition or as one determined by societal influence and behavioural norms.
On a patient level, we must avoid teaching our students and trainees to stigmatise and label based on gendered ideas of normalcy and debunk gender stereotypes in healthcare — for example, that the archetypal patient with an eating disorder must be adolescent, female and fixated on calorie-cutting with a BMI lower than her age, and equally, that it is normal for women to experience significant pain and psychological upheaval due to menstruation.
To champion these initiatives requires further support for more women in clinical academia, research posts and department leads, to translate representation into change.
This approach, despite popular villainisation of the so-called “man-hating feminist”, does not and should not exclude men.
In fact, in direct opposition to this criticism, true feminism benefits everyone, men and women alike, because it is not just women that fall victim to stereotypes and inequity.
For example, erasing the stigma associated with men’s mental health and vulnerability, even in small circles, is essential to reducing the frequency of male suicides, which are particularly abhorrent in the LGBT+ and BAME communities.
Equally, our female-orientated perception of mood and eating disorders further alienates male patients and creates additional barriers to accessing appropriate support.
This complex interaction between biological, social and cultural components that increases risk in these groups is equally reflected in the feminist movement, which seeks to include, understand and recognise the heterogeneity of individuals and their experience. To alter societal expectations of masculinity requires a reciprocal shift to normalise women stepping into more traditionally male-dominated positions of bread-winning, leadership and self-reliance.
By addressing these, it is my hope that psychiatry will remain and develop as a field covered by a diverse and representative array of doctors, who understand and are able to interpret the emotional, psychological and sociological impact of disease on the individual.
Therefore, the future of psychiatry should at every opportunity, be routed in the mantra that the future not be female but be feminist in its thinking.

NOTE FROM THE EDITORS: If you enjoyed today’s blog by Rebecca, be sure to head over to InSPIre the Mind and check out the previous blogs in our Psych Star series covering topics such as compassion, the mind-body interaction, and the future of child & adolescent psychiatry.